Still
SUSAN
TIPS FOR LEWY Body CAREGIVERS

Caregiving
tips include:
Hydration
Pressure Sores
Hygiene
Medications
Hallucinations
Eating
Comforting
Safety
I need
Lewy Body Dementia
caregiving tips for...
Early Stage
Early stage LBD typically begins with cognitive challenges like multitasking, hallucination of animals or people, and motor functions changes such as tremors, balance issues, and rigidity.

Mid Stage
Clear Lewy Body Dementia symptoms become more pronounced, including memory loss, sleep disturbances, behavioral changes, and sundowning.


Late Stage
Need full or partial assistance with all daily living tasks, urinary & occasional bowel incontinence, swallowing problems, worsening behavioral changes, and in some cases, immobility.


End Stage
At this stage, your loved ones will lose their ability to communicate, have swallowing problems, and difficulty recognizing family members. They will not be able to walk and require round the clock assistance.

Welcome!
Sorry you're here
If you found this site, I'm sorry. Sincerely, deeply sorry that your loved one is also suffering from Lewy Body Dementia.
Still Susan was created in honor of my wonderful mother, Susan, for full-time caregivers - like you & me - as a quick resource of curated tips, thoughtful hacks, and useful products.Our mission is to help you navigate LBD at every stage of this difficult caregiving journey with your loved one. And to support you in providing care filled with love, patience, compassion, and dignity. Because they're STILL your loved one, and always will be. It's the one thing Lewy Bodies can never change.
About
Still Susan
Still Susan was created as a tribute to my mom, Susan, who was diagnosed with Lewy Body Dementia in 2018. This disease is not something I would wish on anyone, let alone the best, most lovable human I have ever known.
Extremely wise, warm, witty, creative, accomplished. Susan is all of these things, and so much more. But my mother's superpowers have always been her kindness and empathy, even towards strangers. While Lewy Body Dementia isn't the ending she wanted or deserved, she’d enjoy knowing that her path could help lessen someone else's pain.
With that said, my fellow caregivers, I hope this website of tips I've learned as her daughter and full-time caregiver make your stressful, exhausting, and heartbreaking road a little easier. For both you and your loved ones with Lewy Body Dementia. ♡
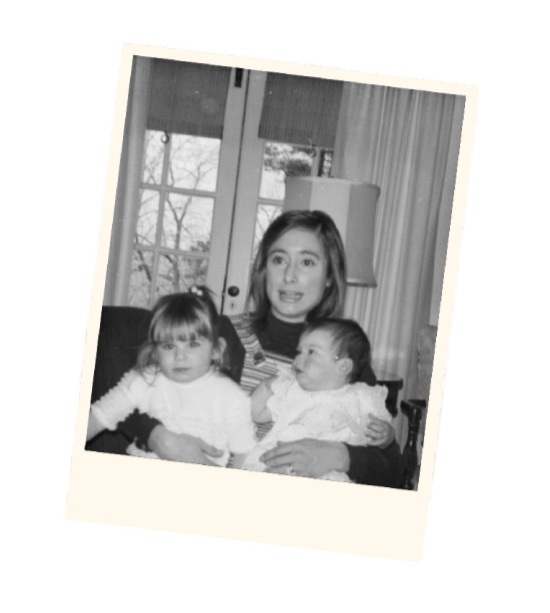
My mom, Susan
The real Susan
While I wanted to be respectful of my mom's privacy and use illustrations,
I don't think she'd mind me sharing this ONE picture with "her girls"
. . . and her biggest fans.
A Huge
Thank you
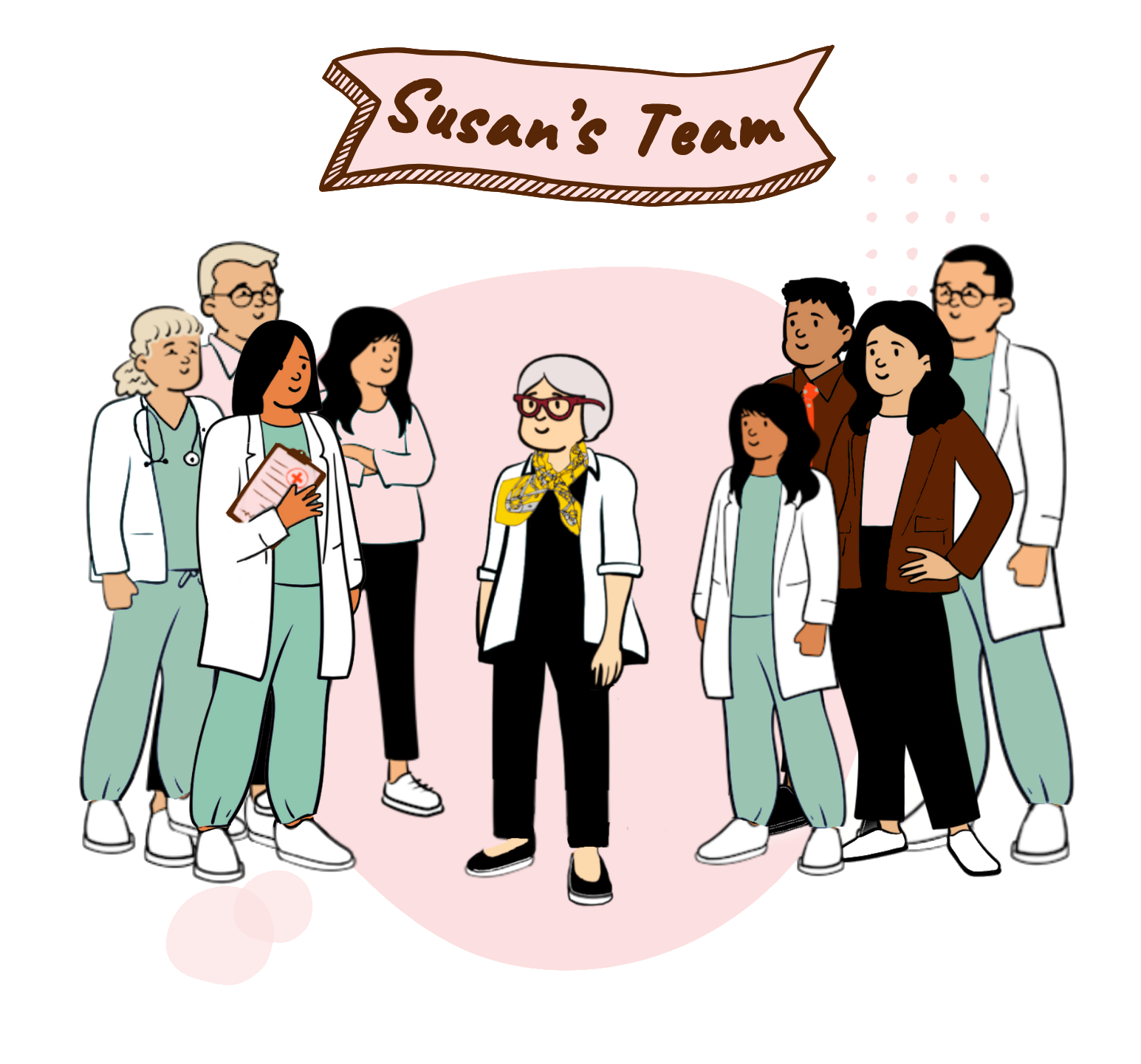
My mother is fortunate to have a wonderful medical team managing her Lewy Body Dementia. Throughout every phase of her journey, their expertise, quick responsiveness, and compassion have made a significant difference. Our family will be forever grateful for their exceptional care and they deserve to be recognized for being outstanding professionals.
Susan's Medical Team
Dr. Michal Gostkowski, DO (Neurology)
Dr. Era Hanspal, MD (Neurology)
Dr. Rashmi Jain, MD (PCP)
Dr. Naveed Khokhar
Rachel Lovati, PT, DPT
Christine Nelson, CNS
Dr. John Sanitato
Megan Scott APRN, CNP
(L to R) Megan Scott, Dr. John Sanitato, Dr. Rashmi Jain, Rachel Lovati, Mom, Dr. Era Hanspal, Dr. Naveed Khokhar, Christine Nelson, and Dr. Michal Gostkowski
Contact
Submit
YOUR TIP
Hi! If you’re a caregiver for someone with Lewy Body Dementia, your tips could be incredibly valuable to others who are dealing with similar issues or looking for new solutions.Whether it’s advice on managing tough behaviors, creative problem-solving, or a product that has worked well for you, your insights can greatly support the LBD caregiving community and their families.Please keep your tip clear and concise, and if you’re recommending a product, include a link for us to review.
Thank you for helping
the LBD community!
♡S.S
Legal
DISCLAIMERS
By accessing this website, you acknowledge and accept the terms and conditions outlined below. If you do not agree with these terms, you must refrain from using this website.
Medical Disclaimer
This website is offered solely for educational and informational purposes and does not constitute providing medical advice, diagnosis, treatment, or professional services. The information presented on Still Susan is not intended for diagnosing or treating any health condition or disease. Individuals seeking personal medical advice should always consult a licensed healthcare professional.You should always consult your doctor or another qualified health provider about any medical concerns. Do not disregard or delay seeking professional medical advice based on information contained on Still Susan’s website.If you think you may have a medical emergency, call 911 or proceed to the nearest emergency room without delay. The use of this website does not create a physician-patient relationship. Neither Still Susan, its employees, nor any contributors to this website make any representations, whether express or implied, regarding the information provided herein or its application.
Copyright Disclaimer
All content on "Still Susan" is the property of the website owner and is protected by copyright laws. Unauthorized use or duplication of this material without written permission from the website owner is strictly prohibited. Excerpts and links may be used, provided that full and clear credit is given to "Still Susan" with appropriate and specific direction to the original content.
Lewy Body
RESOURCES
Lewy Body Dementia is the second most common form of progressive dementia after Alzheimer’s disease, and yet, dedicated Lewy Body resources are still difficult to find.Below are a few LBD non-profit organizations, websites, and podcasts to check out. And, if you can, send a little donation to the non-profits to support their important work.
Lewy Body Dementia
Resource Center
Words cannot express how invaluable The Lewy Body Dementia Resource Center (LBDRC), is to those living with Lewy Body Dementia and their caregivers.
Run by Norma Loeb, the LBDRC is a charitable 501(c)(3) non-profit organization, which offers support groups, a LBD Helpline (Monday-Sunday: 8am to 8pm), and a treasure trove of informative content on their website from specialized Lewy Body doctors, experts, and experienced caregivers.
Website: lewybodyresourcecenter.org
Helpline: 516-218-2026 or 833-LBD-LINE
Lewy Body Dementia
Association
The Lewy Body Dementia Association (LBDA) is the leading national organization dedicated to improving the lives of those living with Lewy body dementia (LBD), the second most common form of neurodegenerative dementia affecting approximately 1.4 million people in the United States alone.Established in 2003, LBDA’s mission is to optimize the quality of life for those affected by LBD by accelerating awareness, advancing research for early diagnosis and improved care, and providing comprehensive education and compassionate support.
Website: www.lbda.org
Helpline: 888-539-9767
The Lewy Body
Society
The Lewy Body Society is a UK-based charity organization that aims to raise awareness, support individuals and families affected by Lewy Body Dementia, and fund research into the disease. Established in 2006, the society provides information, resources, and guidance for those living with or caring for someone with Lewy body dementia. Their mission is to ultimately improve the quality of life for those impacted by this challenging neurodegenerative disorder.
Website: www.lewybody.org
Lewy Body
Canada
Our friendly neighbors up North have established a valuable online resource for those impacted by Lewy Body Dementia (LBD). Founded by Timothy Hudson, a former caregiver to his mother, Lewy Body Canada serves as a non-affiliated platform offering a wealth of information and insightful articles designed to assist individuals and their loved ones in navigating the complexities of Lewy Body Dementia as best they can.
Website: www.lewy.ca
Dementia Coach
Diane
Diane Chew is a breath of fresh air for caregivers in the LBD community. She is a certified life coach and full-time caregiver for her sweet husband, Ben, who has Lewy Body Dementia. Diane shares her experiences, tips, and insights on social media to help other caregivers with dementia care. She also offers a caregiver newsletter and group coaching services, beginning Fall 2025.
Website: dementiacoachdiane.com
Newsletter: click here to sign up
Lewy Body
Roller Coaster
A podcast for Lewy Body Dementia patients and their families. You will hear firsthand, the ups and downs and twists and turns of Lewy Body Dementia from families directly affected as they share their support and experiences on all things Lewy Body.
Website: www.lewybodyrollercoasterpodcast.buzzsprout.com
Lewy Body
Life
Lewy Body Life helps care partners, family and friends understand and navigate the often complex and unpredictable Lewy Body Dementia (LBD) journey. Here real people with real experience and real insight share essential information for caring and coping. They also guide you to professional resources, strategies and support networks that can help increase awareness and understanding of LBD and aid you in your LBD journey.
Website: www.lewybodylife.com
Like Susan's Shirts?
Well, you have excellent taste. Plus all proceeds from your sale will be donated to a Lewy Body non-profit.
Still Susan is for informational & educational purposes only (see disclaimer)
Free Caregiver
downloads
Caring for your loved one with Lewy Body Dementia can be quite challenging, but we’re here to help! We invite you to download our free PDFs to make things a bit easier for you.
Sign up to get quarterly Lewy Body Dementia caregiving tips straight to your inbox.
Caregiving
PRODUCT LISTS
Susan has always loved lists to keep her busy life organized. For your convenience, below are lists of some products, foods, and personal care supplies for each stage of caregiving so you'll know what you'll need to help your loved one.
Early Stage
Products links with an asterisk (❋) are mentioned in Quick Reads and Instant Tips
Products
Labels for kitchen and bedroom
Smart TV
Foods
Avocados
Blackberries
Blueberries
Broccoli
Brown Rice pastas
Brussels Sprouts
Chicken
Coconut Oil
Fish
Ginger
Green Tea
Ice Cream (any flavors)
Kale
Kefir (Lifeway)
Kiwi
Mixed greens
Pistachios
Prune Juice
Raspberries
Spinach
Strawberries
Yogurt (Oui is Mom's favorite)
Personal Care
AREDS-2 Supplements (for vision)
Dental Floss picks
Fish Oil supplement
Interdental Cleaners (like Dentek Easy Brush)
Magnesium supplement
Mouthwash
Multivitamins
UTI Home Testing Kits
Vitamin B12
Vitamin D3
Mid Stage
Products links with an asterisk (❋) are mentioned in Quick Reads and Instant Tips
Products
Serving Trays (small, medium & large)
Vive Alternating Air Pressure Mattress Pad for bed sore prevention ❋
Foods
Avocados
Blackberries
Blueberries
Broccoli
Brown Rice pastas
Brussels Sprouts
Chicken
Coconut Oil
Eggs
Fish
Ginger
Green Tea
Ice Cream (any flavors)
Kale
Kefir (Lifeway)
Kiwi
Mixed greens
Prune Juice
Raspberries
Spinach
Strawberries
Yogurt (Oui)
Personal Care
AREDS-2 supplements (for vision)
Arnica Gel (for muscle stiffness)
Baby Wipes
D-Mannose supplement (UTI prevention)
Dental Floss picks
Dry Shampoo
Fish Oil supplement
Interdental Cleaners (like Dentek Easy Brush)
Magnesium supplement
Mouthwash
Multivitamins
Probiotic Supplement
UTI Home Testing Kits
Vitamin B12
Vitamin D3
Late Stage
Products links with an asterisk (❋) are mentioned in Quick Reads and Instant Tips
Products
Blender
Clamp Lamps (for extra lighting) ❋
Hand Blender
Humidifier
Vive Alternating Air Pressure Mattress Pad for bed sores ❋
Foods
Acorn Squash (mashed)
Applesauce
Avocados (mashed)
Butternut Squash (mashed)
Cottage cheese
Finger Foods (see full list)
Fruit (peeled and pureed)
Hummus
Ice Cream (smooth, no chunks)
Jello
Kefir
Oatmeal (pureed)
Outshine Fruit Bars
Pound Cake (for weight gain)
Prune Juice
Pudding
Smoothies
Slushies
Scrambled eggs
Soups (pureed)
Sweet Potatoes (mashed)
Yogurt (Oui)
Personal Care
AREDS-2 supplements (for vision)
Arnica Gel (for muscle stiffness)
Baby Wipes
Dental Floss picks
Dry Shampoo
Enema
Epsom Salt
Fish Oil supplement
Interdental Cleaners (like Dentek Easy Brush)
Lotion
Magnesium supplement
Mouthwash
Multivitamin
Probiotic supplement
Suppository
UTI Home Testing Kits
Vicks Vaporub ❋
Vitamin B12
Vitamin D3
Zinc Oxide cream (like Desitin) ❋
End Stage
Products links with an asterisk (❋) are mentioned in Quick Reads and Instant Tips
Products
Blender
Hand Blender
Shampoo Basin
Foods
Acorn Squash (mashed)
Applesauce
Avocados (mashed)
Butternut Squash (mashed)
Carrots (pureed)
Cottage cheese
Cream of Wheat
Fruit (peeled and pureed)
Hummus
Ice Cream (no chunks)
Jello
Kefir
Oatmeal (pureed)
Pedialyte Hydration Drink
Pedialyte Freezer Pops
Prune Juice
Pudding
Rutabaga (mashed)
Smoothies
Scrambled eggs
Soups (pureed)
Sweet Potatoes (mashed)
Yogurt (creamy only, no fruit chunks)
Personal Care
Baby Wipes
Colace ❋
Disposable Nitrile Gloves
Dry Shampoo
Enema
Epsom Salt
Lotion
Mouthwash
Suppository
UTI Home Testing Kits
Zinc Oxide cream (like Desitin)

Love a product?
We want to know
about it!
Sign up to get quarterly Lewy Body Dementia caregiving tips straight to your inbox.
Early Stage
Lewy Body Caregiver Tips
Quick Reads
Click on a post for Lewy Body Dementia caregiving tips in under three minutes.

Things you shouldn't say
to a loved one with LBD
4 critical things to do
after a loved one’s
Lewy Body diagnosis
Simple ways to organize
pills and stay on schedule
How to keep the home
safe in early stage Lewy
Body Dementia
FREE DOWNLOAD
Kitchen labels for Lewy
Body Dementia
Easy dinner recipes to
drop off and freeze
for a loved one with
Lewy Body Dementia

Instant Tips
Tap or scroll over to view some fast Lewy Body caregiving tips.

Lewy Body Dementia
can show up in different
ways, such as:
• memory problems
• problems multitasking
• hallucinations
• difficulty staying focused
• sleep issues
• acting out dreams
• tremors
• balance issues / falls
Someone with cognition
problems shouldn't attend
doctor's visits alone. Call
in remotely if you can't
go in person.
If you meet resistance, tell
your loved one you want
to support them (you do!)
or offer to take notes.
• Get an Amazon Echo; go
to "Reminder" to set daily
pill announcements
& phone notifications
• Set reoccurring pill
alarms on their phone
• Use "Dose Reminders" on
the Apple Heath app
Pinch the skin over the
back of the hand or lower
arm so that it is tented up
& hold for a few seconds.
This will show skin turgor.
Mild dehydration will
cause the skin to be
slightly slow in its return to
normal.
Hallucinations can be
pretty harmless at first.
Animals, babies, and
sometimes little humans
are typical.
If your loved one is seeing
scary hallucinations,
speak to their doctor
about medications to take.
Cost Plus Drugs is a
great resource for
cheaper LBD meds.
- AND -
If only a specific (and
pricier) drug will work,
call their RX plan and ask
how to qualify for a
Tier Exemption.
People with LBD are very
sensitive to medications.
Here are a few things to
watch out for when
trying a new pill:
• Vomiting
• Constipation
• Diarrhea
• Excessive sleepiness
• Abnormal Behavior
• Paranoia / Delusions
To prevent slips or falls in
the shower, try using:
• Slip-On Water Shoes
• Non-slip shower mat
• Plastic shower chair
⚠️ Avoid buying shower
handles with suction.
They tend to slip. ⚠️
Buy a 40oz Owala
insulated water bottle
with a handle. Fill it 2x/day.
-OR -
Keep a 64oz jug of water
in fridge so they know how
much they need to drink
every day.
Have them take a picture
of the hallucination with
their cell phone to
determine whether or not
it's real.
A "File of Life" is a form with
a magnet that goes on the
refrigerator that provides
vital medical information
to first responders.
"File of Life" is free through
your local fire, police, or
ambulance department.
When more than one
medication is started or
changed at the same
time, it can be difficult
to determine if a new
side effect or problem
is due to one drug or
another.
Helpful Links
Articles and tutorial videos to help you tackle common LBD caregiving problems.
Where to next?
Got a good tip?
We want to hear
from you!
Sign up to get quarterly Lewy Body Dementia caregiving tips straight to your inbox.
Mid Stage
Lewy Body Caregiver Tips
Quick Reads
Click on a post for Lewy Body Dementia caregiving tips in under three minutes.

Lewy Body Dementia
caregiver tips for doctor's
appointments
Best TV shows and movies
for people with Lewy Body
Dementia
Ways to use Alexa for
Lewy Body Dementia
caregiving
Tips to manage sundowning
for Lewy Body Dementia
FREE DOWNLOAD
Make your own daily
pill schedule PDF templates
for Lewy Body Dementia
Fidgeting strategies &
activities for Lewy Body
Dementia
Instant Tips
Tap or scroll over to view some fast Lewy Body caregiving tips.

Try using acupressure on
the webbing between their
thumb and index finger to
relieve anxiety.
Gently rub the spot
between their thumb and
forefinger and then hold
the position for a moment.
Repeat as needed.
• Haloperidol (Haldol)
• Fluphenazine (Prolixin)
• Chlorpromazine
(Thorazine)
These antipsychotic meds
are known to worsen
neuropsychiatric and
motor symptoms
including cognition and
psychosis, and could
result in death.
The Nova Zoom Rollator
It's sturdy & lightweight,
has responsive brakes,
& big wheels that don't
get caught on curbs.
It's a tad pricey, but their
safety is worth it.
Put a bed alarm pad
on the floor to alert you
when they step out of bed.
You can also tape a
wireless driveway alarm
to the bedpost so you
know when their feet are
dangling over the side
before they hit the floor.
To quickly calm your
nervous system, tilt your
head to the right side
toward your right shoulder.
Rest it there and just wait...
eventually, you'll let out a
BIG yawn & feel your body
relax.
Now do the left side.
Repeat as needed.
Non-verbal cues can
reveal a lot to someone
with Lewy Body Dementia.
Set a positive mood by
speaking to your loved
one in a pleasant and
respectful manner, and
smiling as much as
possible.
Remain calm and call 911
for a non-emergency
lift assist.
🚨Don't pick them up
yourself. You can't caregive
if you're injured.🚨
Costco!
Their Hearing Aid Center
& Optical department are
super affordable and
have excellent service.
Typically, it means they
are not feeling safe or
they're uncomfortable.
D-Mannose
We use the "Now" brand
and mix 1 teaspoon
of the powder into a glass
of prune juice every
morning.
Once you've confirmed a
pill works for your loved
one, ask their doctor for a
90-day prescription to
save yourself several trips
to the pharmacy.
Tip from Holly U.
Whether it’s a big ask or a
small one, simply say
“Now is not a good time.”
No need to over explain
or even give an excuse.
This should be enough.
Helpful Links
Articles and tutorial videos to help you tackle common LBD caregiving problems.
Where to next?
Got a good tip?
We want to hear
from you!
Sign up to get quarterly Lewy Body Dementia caregiving tips straight to your inbox.
Late Stage
Lewy Body Caregiver Tips
Quick Reads
Click on a post for Lewy Body Dementia caregiving tips in under three minutes.

How to clean urine out of
couch, carpet, bedding, and
mattress
How to handle common
Lewy Body Dementia
behavioral problems
Pressure sore prevention for
Lewy Body Dementia
Tips to manage incontinence
for Lewy Body Dementia
Types of finger food
to eat for late stage
Lewy Body Dementia
FREE DOWNLOAD
Laundry stain remover
guide for Lewy Body
Dementia caregivers
Instant Tips
Tap or scroll over to view some fast Lewy Body caregiving tips.

4 to 8oz of prune juice a
day should do the trick.
If still having trouble,
see "Acupressure for
stomach ache & painful
pooping" video in "Helpful
Links" below.
Signs may include difficulty
urinating, change in urine
smell, darkening urine color,
& fever.
However, some UTIs
present without ANY clear
symptoms, so also look out
for profound behaviorial
changes, balance issues,
& excessive sleepiness.
Use a Goody Half-Claw
Hair Clip to secure the
straps in the back to prevent
the mask from slipping off.
1) Get a fly swatter
2) Swat at objects where
they're looking & say
something like "okay, it's
time to leave."
3) Go to any door, say
"don't come back" & slam it
4) Comfort your loved one,
and ask if they're ok
Put a frozen bag of peas or
an ice pack on the back
of their neck.
Green is considered calming
and can reduce central
nervous system activity.
Blue is also calming & can
reduce anxiety, and dark
blue decreases appetite.
Black is perceived as scary
or intimidating, especially
below the knees.
Put a pillow under your knees
when you sleep.
Also, if you have the time, try
Lower Back Love from Yoga
with Adrie.
Electric blankets make it
too easy for them to get
overheated and confused.
Use a weighted blanket
instead or put a blanket
in the dryer to warm it up
for some quick soothing.
Under the desk stationary
bike peddles.
Sit your loved one in a safe,
comfy chair, put on music, &
have them peddle for a few
minutes.
You can assist, if
needed, by gently pushing
their knees or tips of their
toes down as they peddle.
When you see a red spot:
1) Smear some petroleum
jelly over it with a clean finger
2) Cover it with non-stick
pad with adhesive tabs
3) Secure with paper tape
4) Repeat daily until red spot
disappears
5) Call doctor if redness
increases
• Use a sliding shower chair
& a hand-held shower head
• Start at feet & work up
• Do hair last, use a washcloth
to wet & rinse hair
• Keep shirt or towel on for
modesty; remove when wet
• Wrap them in a warm towel
from the dryer when done
Our purpose as caregivers
is to provide comfort, support,
& empathy, so it's important
to go along with their
perception of reality.
Correcting them will only
bring them shame, frustration,
agitation, & erode their trust
in you.
Walmart has a
caregiving brand called
"Equate" which is super
cheap.
As an added bonus,
they deliver!
While your loved one may
not communicate, they still
understand what you say.
Explain this to visiting
family & friends to avoid
this hurtful, disrespectful
faux pas from happening.
Put some Vicks Vaporub
on both sides of the temple
for fast relief.
Helpful Links
Articles and tutorial videos to help you tackle common LBD caregiving problems.

8 practical tips to help
someone with dementia
to eat more
Reduce dementia-related
swallowing problems.
Swallowing can be
a killer. Be vigilant.
7 ways to reduce &
manage mean dementia
behavior
How to help someone
with Alzheimers or
Dementia who is
experiencing
hallucinations
Acupressure for stomach
ache & painful pooping
The role of palliative and
hospice care in lewy body
dementia
Helping a patient into bed
What to say when a loved
one doesn’t recognize you
Where to next?
Got a good tip?
We want to hear
from you!
Sign up to get quarterly Lewy Body Dementia caregiving tips straight to your inbox.
End Stage
Lewy Body Caregiver Tips
Quick Reads
Click on a post for Lewy Body Dementia caregiving tips in under three minutes.
Instant Tips
Tap or scroll over to view some fast Lewy Body caregiving tips.

Use an insulated
food container.
.
1) Get a fly swatter
2) Swat at objects where
they're looking & say
something like "Okay, it's
time to leave."
3) Go to any door, say
"Don't come back" & slam it
4) Comfort your loved one,
& tell them they're safe
Put an Always Maxi Extra
Heavy Overnight Pad
where the sore is located
for some relief.
Use paper medical tape
to affix properly if needed.
For bottom sores, stick
pad on the outside of
their incontinence pants.
Constipation and
dehydration.
• Joy For All interactive
companion pet cat
• A weighted blanket
• Friendly Cuddle weighted
lap blanket
Assurance Incontinence
Unisex Stretch Briefs
(with tabs) from Walmart's
Equate brand.
• Put a rolled up washcloth,
ace bandage, or craft
cone into their fist
between their thumb and
index finger to separate
their hand and give relief.
• See "Helpful Articles"
below for palm massage.
• Ask their doctor about
botox injections.
Blend in:
1-2 tablespoons of
cocoa powder
- OR -
2" slice of pound cake
Some meds are available
in orally disintegrating
tablets (ODT) or liquid
form.
Also, ask your doctor if
capsules can be opened
and sprinkled on to yogurt
or apple sauce.
Helpful Links
Articles and tutorial videos to help you tackle common LBD caregiving problems.
Where to next?
Got a good tip?
We want to hear
from you!
Sign up to get quarterly Lewy Body Dementia caregiving tips straight to your inbox.
Still Susan's
LBD Shop
Want to look sharp, build LBD awareness, and give back to Lewy Body Dementia non-profit resources we all need? Perfect! You've come to the right place.
Things you shouldn't say to a loved one with Lewy Body Dementia
Communication with someone who has Lewy Body Dementia should be patient, respectful, and compassionate. By avoiding these phrases, you can create a more supportive and understanding environment for them instead of potentially triggering confusion, anger, frustration, or distress.
"Do you remember...?"
It should go without saying, but you shouldn’t ask someone with cognition issues if they “remember" anything - including you.It's a hard habit to break, but for your LO's sake you really should try. Not only does this phrase make them feel pressure to remember, but it also leaves them feeling embarrassed, sad, or frustrated when they can't.Instead, begin the sentence "I remember when..." or "I remember you telling me about...." so you can reminisce without putting them on the spot. You should also introduce yourself when you enter their space during the later stages. If my mom greets me with a "Hi, darling (or sweetie)" and her sweet smile, then I know she remembers me.
"No, you're wrong."
Try not to argue with them. It's not a fair fight for someone with cognitive issues. Besides, there's no benefit to pointing out they're wrong, and it will only escalate their frustration and agitation.
"There's nothing there."
Hallucinations are a big part of Lewy Body Dementia. They are VERY real to your LO, so it's best not to contradict or question what the person is seeing. It will only agitate them further, and your goal is to deescalate the situation.Instead, acknowledge what they see. And, if the hallucinations seem to be scaring your LO, try to empathize with their feelings and provide reassurance that they're safe. Taking them to another room often helps, too.
"What do you want to do today?"
Open-ended questions can be quite challenging for someone with LBD. They might cause confusion and frustration, resulting in no response at all.Instead of asking open-ended questions, consider being more direct by suggesting activities like "Let's go for a walk," or limit choices to no more than two, such as "Do you want Butter Pecan or Chocolate ice cream for dessert?" instead of asking what they want for dessert.
"Calm down."
Your LO with Lewy Body Dementia is coping with anxiety, frightening hallucinations, and behavioral changes every day, all of which are beyond their control. Telling them to "calm down" is the least helpful thing you could say as it can come across as belittling, dismissive, and devoid of compassion.Instead, try to identify why they're upset (scared, frustrated, etc.,), acknowledge and validate their feelings, and offer them your support. You're on their team, remember? Let them know you are by making them feel heard and understood.
"I just told you that."
As frustrating as this may be, try to remain calm and answer the question like it's the first time they've asked. You don't ever want to make your LO feel shamed or embarrassed for having a disease.
"Why are you being so difficult?"
It's important to always remember that they're not being difficult on purpose - and it's never personal - so keep calm and don't get frustrated. Otherwise, you run the risk of escalating the situation and making it worse.Try to identify what’s triggering their mood and address their needs. Are they in discomfort? Scared? Do they need some food? Was it something you said or did? Clearly something is wrong, and I trust you'll do your best to figure it out.
"They passed away years ago."
Whether it's a parent, spouse, loved one, or a favorite pet, it's best to avoid mentioning that they have passed away.It's natural to feel conflicted about not telling the truth, but consider it a compassionate act instead. Bringing up a loss could only bring more pain to your LO with Lewy Body Dementia, something you'd never want to do.So, the next time your LO asks about someone who has passed away, go along with it and say they're out and will return soon. Even better, use it as an opportunity to reminisce, which will likely bring comfort to your LO since this person (or pet) is clearly on their mind.
You may slip up from time to time....
and that's okay.
♡S.S
You might also like
4 critical things to do after a loved one's Lewy Body diagnosis.
Your head is probably spinning after your loved one was diagnosed with Lewy Body Dementia. I get it, mine was, too. So I decided to jot down some critical things that need to get done at this stage to make caregiving for your loved one easier.
1. Get their POA & Advance Directives
End-of-life documents can be a sensitive topic for people, so your LO may not have them. However, it is essential get these documents completed promptly, especially while your LO is still able to make these decisions and sign the necessary paperwork. Don't delay in ensuring their wishes are known and honored.Although it varies by state, you'll need some (or all) of these documents:
Durable Power of Attorney
Health Care or Medical Power of Attorney
Do Not Resuscitate (DNR) directives
Living Will
If your family doesn't have a lawyer, you can sign up for LegalZoom or Legal Shield for a small monthly fee of around $30/month.Once you have these documents, you'll need to provide copies to your LO's doctors, pharmacy, bank, financial institutions, etc., to speak on their behalf.
2. Set up their EHR account
Electronic Health Record (EHR) systems like MyChart make it so easy to handle your LO's medical affairs. From making appointments, accessing test results, renewing prescriptions, and messaging their doctor with urgent questions, it's an efficient way to manage their health.Make sure you write down their username & password and keep it in a safe place.
3. Line up their doctors
Having a good healthcare support team is priceless when dealing with a condition such as Lewy Body Dementia. How you manage Lewy Body Dementia as the disease progresses makes all the difference. Make sure to do your research, get referrals, and read online reviews before selecting their doctors.Your LO will need some or all of the following specialists to manage LBD:
Neurologist and/or Neurogeriatrician
Speech-Language Pathologist
Geriatric Psychiatrist (for support, plus depression & anxiety medications)
Physical Therapist (especially if your LO has Parkinsonian symptoms)
Also be sure your LO's current Primary Care physician is familiar with Lewy Body Dementia, extremely responsive, and easy to work with. Shout out to Dr. Jain and her team at the Cleveland Clinic who've been amazing for all of Mom's little emergencies that pop up!
4. Set up their online accounts
You've probably already noticed by now that your LO needs help managing their lives. It's best to sit down with them and create online accounts since you -- or someone else -- will be making sure their life run smoothly.
Monthly bills (utilities, cable, cell phone, car payments, credit cards, mortgage payments, car & home insurance, etc.)
Health Insurance company & Medicare account
Online banking (to pay monthly bills)
Retirement & Investment accounts
Pharmacy (to order meds)
Create a family gmail account(optional)*
Create a master list of usernames, passwords, security questions, account #'s, and any other info needed for these accounts, and put the list in a safe place.
*A family gmail account is optional, but it's a great way to keep multiple family members informed on important emails & pitch in when needed on any tasks. You can also set pill & appointment reminders remotely to your LO's phone. Another benefit of creating a new gmail account is that it also avoids the awkwardness of asking your loved one for access to their email, and making them feel like they have no control.
It's a lot, but you'll get it done in due time.
♡S.S
You might also like

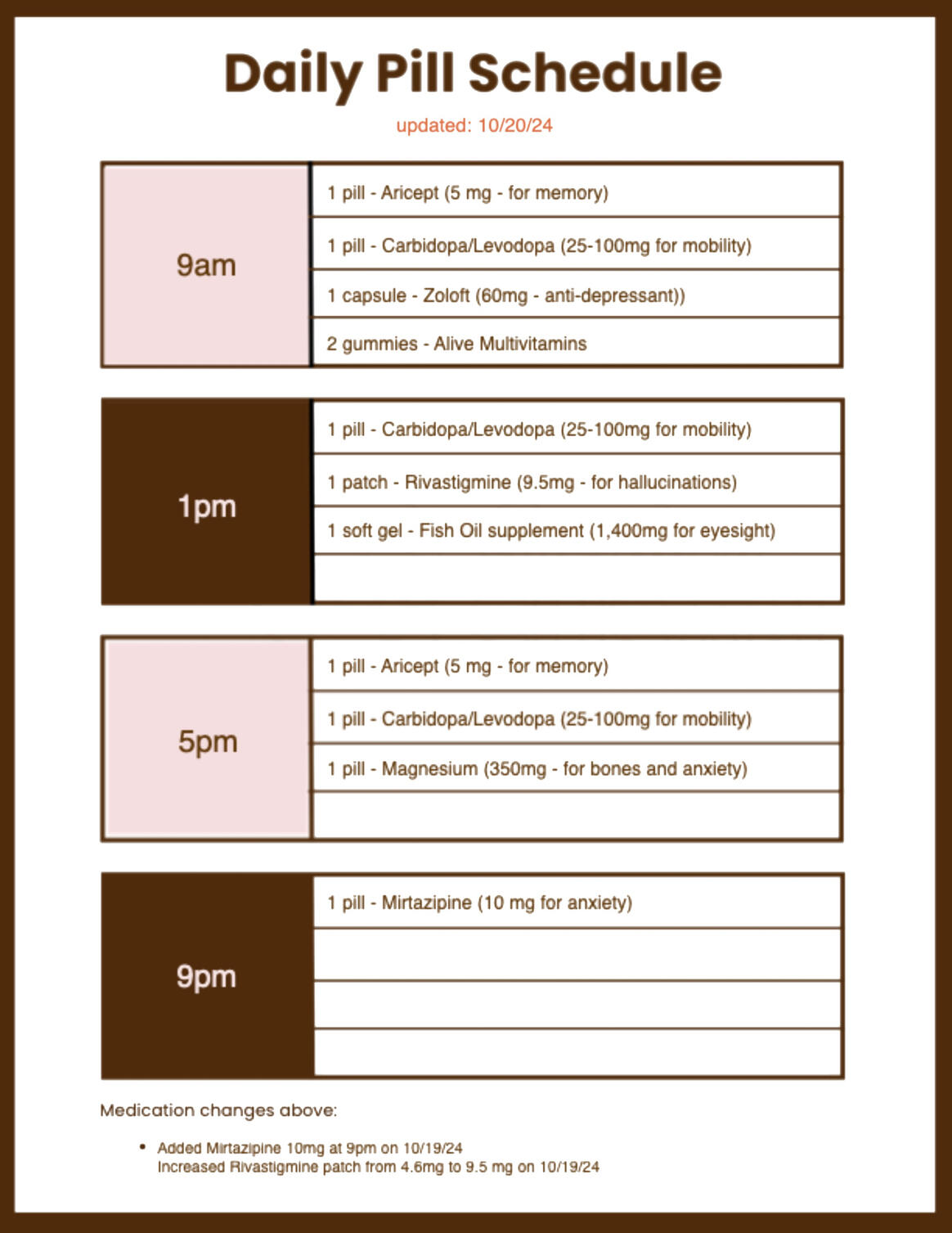
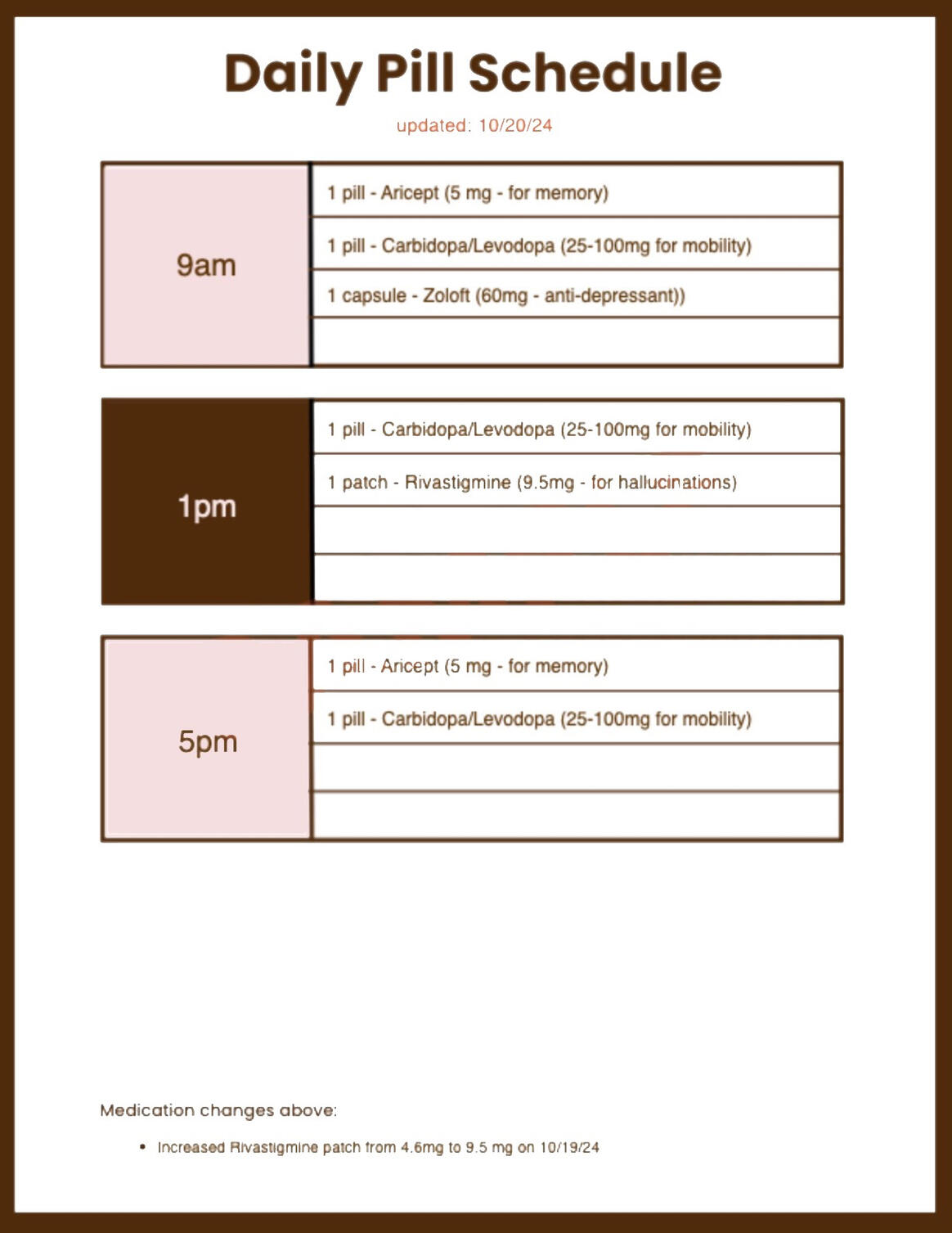
Simple ways to organize pills and stay on schedule
Lewy Body Dementia patients often struggle with organizing & remembering to take their pills as their cognitive function declines. However, there are some strategies that to help caregivers manage this task for their loved ones.
Organize their pills
Every caregiving situation is unique, and it's important to choose a pill management system that is customized for you and your LO's needs and capabilities.
Here are some questions to help you narrow down what you & your LO will need at their current stage of LBD:
How many pills do they take?
How big are the pills?
How many times a day do they need to take pills?
Do the pills need to be portable or is your LO home-bound?
Can your LO correctly sort the pills or does someone else need to do it?
Can your LO correctly take their pills or does someone else need to help them?
Once you have your answers, here are some good pill organizing options to consider:
PILL BOXES
AUTOMATIC PILL DISPENSER
PILL DELIVERY SERVICES*
*Two caveats to consider for PilPack & divvyDOSE is that controlled substances (like Clonazepam, for example) require a signature on delivery in some states and come in a separate bottles, not the pack.
Set Pill Reminders
Even if your pill organizer comes with an alarm, it's a good idea to have backup reminder for you in case something goes wrong. Several Lewy Body Dementia medications need to be taken at the same time every day to manage symptoms, so it's important to remain on schedule.
Set Alexa reminder on Echo (at home) and smartphone notification (if out)
Set calendar reminders on their smartphone
Use the "Heath" app on your iphone (tutorial here)
Send them pre-scheduled emails
Call or text reminders
Make a pill chart schedule
It's super handy to have an updated pill chart schedule close to their meds for you, a home healthcare aide, or anyone filling in for you. You can even take this chart with you to doctor's appointments, like we used to do.You can download this FREE PILL CHART SCHEDULE from Still Susan and add your LO's details.
Online pharmacy & apps
Get your LO signed up for an online pharmacy account and download their app. All major pharmacies have apps, and they'll be your BFF to save time on refills.
Have a backup plan
You've got a lot on your mind, and we're all prone to forget things, so keep an extra pill box filled with their daily pills in your glove compartment, purse, or backpack.You can also divide their pills by time slot into labeled ziplock bags or unused prescription bottles.Just don't forgot to refill the backup pills if you use a dosage...like I've done a few times. :)
Hope this helps!
♡S.S
You might also like
How to keep their home safe in early stage Lewy Body Dementia
Ensuring the safety of their home in the initial phases of Lewy Body Dementia (LBD) is essential to support your loved one in staying independent, preventing falls, and minimizing any confusion or anxiety.I highly encourage you to hire an Occupational Therapist (OT) if you can to visit your home to assess safety and make personalized recommendations for your loved one. If they are on Medicare, this service may be covered if prescribed by their doctor.Meantime, below are some useful tips for keeping your loved safe at home. Take a deep breath and dive in....and remember, you don't have to do everything all at once.
Kitchen
Remove any throw rugs or mats as they can be major tripping hazards
Make food and frequently used kitchen items easy to reach so a stool is not needed
Consider putting labels on cabinets to help easily identify items
Make sure a non-expired fire extinguisher is kept in an easily accessible location
It's a good idea to install an automatic shut-off device for the stove
Try to keep clutter on countertops to a minimum
Keep medications organized and easily accessible, along with their pill schedule
Remove any sharp objects on countertop and drawers
Keep an undated "File of Life" magnet on their refrigerator in case of emergencies, which you can get for free from their local fire, police, or department of health
Don't forget to have a list of emergency numbers on the refrigerator, preferably on colored paper and laminated for easy reference
Bedroom
Remove any rugs, mats, or furniture which could be tripping hazards
Install nightlights for late night bathroom or kitchen trips
You could also put a flashlight near their bed
Remove any clutter, especially in their eyeline when they're in bed
Make sure all electrical cords are securely fastened and out of the way
A bed alarm alert and/or bed alarm pad is an excellent safety measure to add if you're worried about your LO falling late at night.
Have plenty of lighting in the bedroom to prevent shadows after the sun goes down
Living Room
Keep clutter to a minimum
Remove any unsecured rugs or furniture
Make sure all electrical cords are securely fastened and out of the way
Get rid of furniture with sharp corners or put childproof padding on the corners
Consider cutting up pool noodles and affixing them with tape to furniture legs or sharp corners
Keep a basket or shelf of activities your LO enjoys in an easily accessible area.
Again, make sure their living room has plenty of lighting
Bathroom
Place nonslip mats in showers and tubs
Purchase nonslip bathroom mats for the floor to avoid any falls
Install grab bars in the shower for extra support. Avoid grab bars with suction cups, they tend to slip
Consider adding a grab bar near the toilet or a toilet support rail
Get them a pair of slip-on water shoes for added grip in the shower
Use a plastic shower chair to prevent falls and slips, and install a detachable shower head
Place nightlights in the bathroom and along the path to the bathroom
Other home safety measures to consider
Smart bulbs are a great way to increase lighting in rooms at certain times of the day automatically. Once set up, you can also turn them on remotely.
Install nightlights in all rooms, near stairs, and high-traffic hallways
Scan all other rooms for any potential tripping hazards, including electrical cords and rugs
Make sure smoke and carbon monoxide detectors are properly installed and functional in their home, especially in the kitchen and bedrooms
Adjust water heater to 120°F to prevent scalding from hot tap water
You may want to invest in safety devices like fall monitors, emergency call buttons, AirTags, or GPS trackers to alert others in case of emergencies
A picture phone near their favorite chair might be a good idea for emergency calls and keeping in touch with family and friends
Consider adding Amazon Echos to rooms for pill reminders and drop in calling for you or your LO.
Hope these help
keep them safe!
♡S.S
You might also like
FREE DOWNLOAD
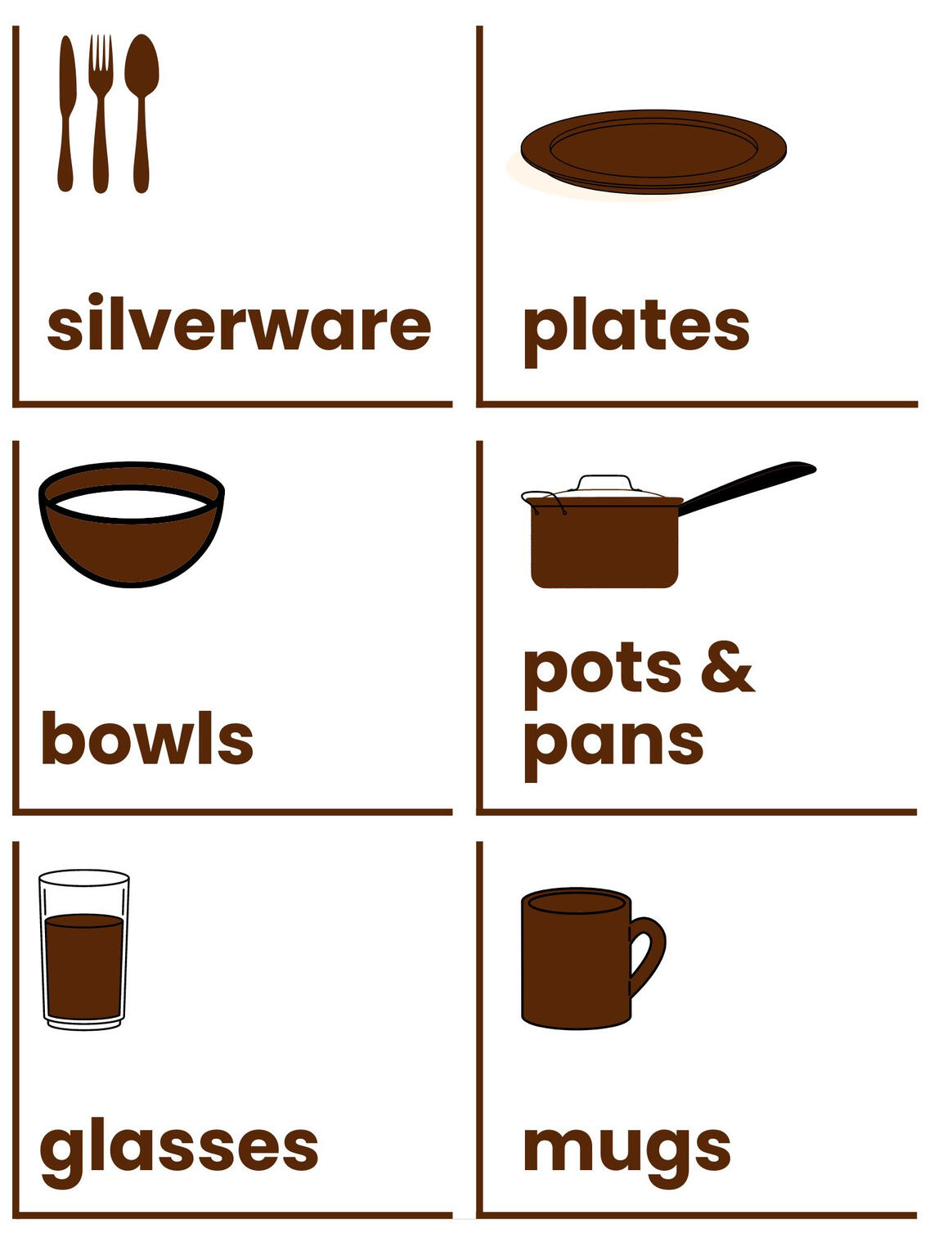
Kitchen labels for Lewy Body Dementia
A great tip for making life a little easier at home for someone with Lewy Body Dementia is to keep things simple and easy to find. Using clear and accurate labels can help reduce confusion and frustration, allowing them to maintain their independence.When my mom was diagnosed with Lewy Body Dementia, my parents made the big move from New York to Ohio so she could get care at the Cleveland Clinic. I was on the hunt for kitchen labels that would help her settle into her new space, but when I couldn’t find any that suited her style, I decided to create my own.Feel free to download these kitchen labels and use them with your loved one!
Download includes:
Instructions
18 Kitchen Labels for cabinets & appliances
Fire Extinguisher sign

Free Lewy Body Dementia
Kitchen Labels
Hope your loved one finds these useful!
♡S.S
You might also like
Easy dinner recipes to drop off and freeze for loved ones with LBD.
Cooking can be quite challenging with Lewy Body Dementia, even if you've cooked like Julia Child for the past 45 years like my mom. One simple way to help out your loved one - and make sure they're eating well - is to fill up their freezer with homemade meals so they don't have to cook.Below are a few fairly healthy and tasty recipes to stash in your LO's freezer. I used to make four of these recipes every two weeks for my parents before becoming Mom's full-time caregiver, which was plenty of food for two people.QUICK TIP:
Divide the meals into microwave-safe Tupperware containers (or ziplock bags) with 1-2 servings in each. This way, your LO (or parents, in my case) can enjoy a variety of meals throughout the week. Also, be sure to write the name of the recipe, reheating instructions, and the date you made it on all of the servings.
Soups
Chicken & Turkey
Beef
Vegetarian
Braised White Beans and Greens With Parmesan (I leave out the fennel, fyi, and mix it with brown rice)
Bon Apetite!
♡S.S
You might also like
Lewy Body Dementia caregiver tips for doctor's appointments
Assuming a more active caregiving role usually means getting more involved in your loved one's medical appointments. As a Lewy Body Dementia (LBD) caregiver, there are some important steps to prepare for a doctor's visit to ensure that the appointment goes smoothly and effectively.Here's a list of suggestions you might want to do before, during, and after their appointment.
Before their appointment
1. Call doctor's office in advance to say you'll be joining your loved one. Find out if your LO needs to sign a consent form or a HIPAA (Health Insurance Portability and Accountability Act) waiver so the doctor can speak with you. If you've also been designated your LO's health care proxy or their Medical/Health Care Power of Attorney, bring the legal documentation with you to the appointment.2. Gather their medical history & medications. Important medical documents, like your LO's medical background, test results, list of medications (including pill allergies), and supplements they're taking will give the doctor a full view of your LO's health and treatment history.3. Write down any changes or new developments in your LO's behavior, memory, or symptoms. For example, is your LO having sleeping problems, seeing more hallucinations, or problems with balance or recent falls? Write down all your observations to discuss them with their doctor. Try to be as specific as possible if you can, and include time of day and any possible triggers or patterns.4. Make a plan for the appointment with your loved one. Prepare a list of questions or concerns you and your LO want to discuss with the doctor about ongoing or recent symptoms, treatment choices, medications, or their care plan. You only have a limited amount of time, so prioritize your questions from most to least important in the event you run out of time. You can always email the doctor later with follow-up questions or any other concerns.5. Ask your loved one if they'd like some one-on-one time with the doctor to speak privately. Remember, it's their appointment, so offer to step out of the room to allow them to have a private conversation with the doctor. Remind them that you're their ally and biggest advocate, and only there to support them. They might decline your offer, but it's a subtle way to show them that they are the ones in control.6. Pack a "go-bag." It’s always a good idea to bring along some essentials to help your loved one feel comfortable while waiting for their appointment! A few bottles of water, some snacks, their medications, and fun activities can really help pass the time and ease any stress. I like to create a playlist of Mom’s favorite songs on my iPad or watch adorable corgi videos that never fail to make her laugh. And if they have any issues with bladder control, don’t forget to pack an extra pair of incontinence briefs just in case.
During the appointment
7. Let your loved one speak: Doctor's appointments can be overwhelming for people with LBD. It's normal to want to help if they're struggling with finding words or remembering details, but doing all the talking might make them feel ignored or belittled. Let them speak for themselves and make sure it's okay with your LO if you chime in occasionally to fill in missing information.8. Record the appointment or take notes. There’s so much information shared during these visits, and it’s easy to miss important details. If your loved one is having trouble with memory and cognition, why not ask the doctor if you can record the appointment? If recording isn’t an option, make sure to write down key information such as treatment plans, medication instructions, test results, and possible treatments. You might find the Wave AI note-taking app super helpful — it creates detailed summary notes, allowing you to remain focused on supporting your loved one.9. Ask for clarification If you don't understand something the doctor says. Don't hesitate to ask for clarification. It's important that you and your LO have a clear understanding of the diagnosis, treatment plan, medication instructions, and care instruction.
After the appointment
10. Treat yourselves to something enjoyable. Appointments can be a bit overwhelming for both of you, so why not plan something fun together afterwards if they’re feeling up for it? Keeping it low-key with a meal or a mani/pedi is always a great option. If they’re a bit worn out and prefer a nap, you could set up something special for later, like going for ice cream or a fun outing with family or friends. Regardless of the choice, you’ve both had a challenging day, and it’s time for a little joy!11. Follow up. Make sure to schedule any recommended tests or specialist appointments for your LO, and mark them on their calendar. Ensure they get their medications and know how to take them. Finally, write down any special instructions for your LO from their doctor and put in a noticeable place.
Hope these tips help!
♡S.S
You might also like
Ways to use Alexa for Lewy Body Dementia caregiving
As a caregiver for someone with Lewy Body Dementia, having an Alexa can be a game-changer in many ways. Here are some ideas on how to use your Alexa to make life easier and more enjoyable for both you and your loved one:
Play music
Alexa can play your favorite songs all day long or some soothing music like "Healing Sounds" to set a peaceful and pleasant vibe for your LO. Music is extremely beneficial when they're feeling agitated, confused, or down, and you can easily manage music from the app, which is pretty convenient if you live remotely.I suggest creating music playlists for various times of the day to match your LO's mood and to save you time. If you're not keen on shelling out for an Amazon Music subscription, you can link your existing music streaming service to your Echo by heading to "Music & More" in the app.Feel free to also use Still Susan's Spotify or YouTube playlists I created for my mom if you don't have the mental energy or time to be DJ.
Set personalized reminders
Use Alexa to remind your LO of important tasks with an announcement, like taking medications throughout the day and upcoming doctor's appointments. This can help your loved one stay organized and ensure that nothing falls through the cracks. Alexa can also send reminders to a caregiver's phone if needed.
Drop-In Calling
Set up voice and video calls (with Echo Show only) with Alexa to help your LO stay connected with family and friends. This can be especially important for those having difficulties using the phone or communicating with others. You can also schedule your drop-in calls around medication and mealtimes to help your LO with these tasks remotely.Remember to be gentle when you drop into voice calls with your LO so you don't scare them or cause a fall. It's a great idea to listen for a moment to see if you can hear them and where they might be. Then, try softly saying "Hello" a few times to catch their attention.
Alexa Emergency Assist
If your LO ever falls or needs emergency help (knock on wood), they can simply say, "Alexa, call for help." In no time, they'll be connected to a trained Urgent Response agent. The agent will organize emergency services, provide crucial health information from your profile to the first responders, and notify your emergency contacts about the situation.For good measure, post a sign near your Echo devices on bright colored paper to remind your LO what to say to Alexa in an emergency.Alexa Emergency Assist costs $7.99 per month, but it seems like a small price to pay for peace of mind.
Control smart home devices
If you've got smart home gadgets and smart plugs, Alexa can help you manage your LO's lights, TV, front door lock, and thermostat without lifting a finger (even remotely, which is handy). This makes it super easy to keep your LO safe and cozy. Plus, you can schedule your lights to come on at specific times using Routines in the Alexa app, which is helpful during sundowners.
Create your shopping list
Keeping track of your grocery list can be a challenge for anyone, especially for busy caregivers! Thankfully, Alexa is here to help. You can easily add items to your shopping list just by using your voice whenever you remember something. Plus, you can choose to add a widget on your iPhone or Android home screen that displays your entire shopping list, making it super convenient while you’re at the store.To get started with the widget, just make sure you have the latest version of the Alexa app installed on your phone.Another fantastic feature is the ability to share your shopping list with friends or family. That way, if someone offers to pick up groceries for you while you're swamped, they can easily see what you need.
Listen to books and podcasts
Alexa can read books from a Kindle and Audible to keep your LO entertained. If it's going too fast, just say, "Alexa, read slower," to slow it down to 75%.You can also enable your favorite podcast service to listen to whatever niche or topics your LO enjoys. We're big fans of Freakonomics Radio, Stuff You Should Know, This American Life, and ArtCurious in our house. And much to my surprise, Who Shat On The Floor At My Wedding? was a big hit with my mom.Try to limit books and podcasts to 10-15 minutes.
Play games
Alexa offers a variety of games that can help stimulate cognitive function and provide entertainment for both of you. Try playing Jeopardy!, Twenty Questions, Song Quiz, or other interactive games through Fun with Alexa.
Hope this makes your life a little easier!
♡S.S
You might also like
Best TV shows and movies for people with Lewy Body Dementia
Struggling with what to watch? We've got you covered. Check out our list sorted by streaming services. And since you're busy caregiving, direct links are included to save you some time.Also, if you're caregiving remotely, check out Jubilee TV which recently launched. It's a tad pricey, but it does allow you to change the channel remotely for your LO, which is huge!
Amazon Prime:
Apple TV+
Basic Cable:
American Idol - on ABC
Dancing With the Stars - on ABC
Pit Bulls and Parolees - Animal Planet
Too Cute - Animal Planet
The Zoo - Animal Planet
Disney+:
Max:
Netflix:
Paramount+
The Smithsonian Channel (Nature's Wonders & Virtual Vacations)
PlutoTV
YouTube
The Best of Red Sea Underwater in 4K - Colorful Reefs & Sea Life + Music
Endless Squirrels and Birds - 8 Hours (Don't knock it - this is highly entertaining!!!)
Flowers Video for Relaxation + Piano Music - 3 HRS | Wooden Shoe Tulip Festival. Episode 2
Relaxing Therapy Music for Stress Relief Anxiety, Memory Loss
Enjoy!
♡S.S
You might also like
Tips to manage sundowning for Lewy Body Dementia
What is sundowning?
Sundowning is when you see changes in your loved one's behavior, typically in the late afternoon or early evening. During this period, the person might feel really anxious, agitated, confused, and have hallucinations or delusions. This could last throughout the night, making it tough for them (and you) to get a good night's sleep.
Potential causes of sundowning
While the exact cause of sundowning is unknown, different variables may contribute to its development, including brain alterations, altered circadian rhythms, exhaustion, and sensory overstimulation.Whatever the cause may be, when the sunlight outside fades and the shadows increase inside, it's very disruptive to your LO's internal body clock, and you may begin to notice a change in demeanor. We call it the "witching hour" in our house, and it's usually when our dear mom struggles the most.
What can make sundowning worse?
Physical discomfort or pain
Shadows
Hunger or fatigue
Anxiety, depression, or other mood disorders
Overstimulation during the day
Disruption of routine
Lack of exposure to sunlight during the day
Vision or hearing impairments
Lack of physical activity
Boredom
Deviation from medication times or missed dosages
Tips for managing sundowning
Closely observe your loved one: The facial expressions and body language of your LO can be quite revealing. If you pay attention, you'll be able to see if they're having a difficult time by their nonverbal cues. More importantly, you can step in to handle any problems before they escalate into bigger ones. For example, if my mom is fidgeting in a chair, that means she restless. If she's staring at a specific spot in the room and her lip is quivering, it's either a shadow or hallucination. You'll begin to noticed patterns in your LO as well, and jump in to handle the situation to make them feel safe and comfortable.
Set a relaxing atmosphere: Play calming music, use aromatherapy, and keep the living space tidy. A cozy chair or sofa by a window can offer a sense of security
Stick to a routine: Aim to follow a consistent bedtime routine, including activities like bathing, brushing teeth, and a quick massage to relax your LO. This can create a feeling of familiarity and security for the person with LBD.
Make sure you have proper lighting: Maintain good lighting in the home at night to decrease the persons disorientation and diminish shadows. We ended up buying a few clamp lamps which don't require table space to increase lighting around the house.
Encourage physical activity: Exercise can help reduce anxiety and improve sleep. A daily walk or gentle stretching can be beneficial.
Keep an eye on medications: Ensure medications are taken correctly and discuss any side effects with a healthcare provider. Some medications can cause confusion, increase hallucinations, or disrupt sleep, so finding the right balance is key.
Cut back on caffeine and alcohol: Both can disrupt sleep, so it's best to avoid them in the evening.
Offer reassurance and comfort: Provide physical touch like hugs or holding hands, and use gentle, comforting words to help the person feel calm and safe. "You are safe here," is a phrase often used. A favorite blanket or mechanical pet can also bring comfort.
Stay patient and positive: Remember, sundowning can be tough for both the person with LBD and the caregiver. Keeping a positive attitude and being patient can make a big difference in handling these challenging moments.
"This too shall pass,"
as Susan would say.
♡S.S
You might also like

FREE DOWNLOAD
Make your own daily pill schedule PDF templates for Lewy Body Dementia
When your loved one is dealing with Lewy Body Dementia, having a daily pill schedule chart to manage medications and supplements is crucial for symptom management and overall quality of life.A simple daily pill schedule chart can help keep track of different medications, doses, and timing to avoid any confusion or missed doses. It allows your LO and their caregiver to see at a glance what needs to be taken when, ensuring consistency and effectiveness of treatment.Feel free to download one of these simple, large print, editable templates I made for my mom. As you'll find, you'll be making updated pill schedules often, so this format makes it easy for you.And don't forget to print extra copies to bring along to doctor's appointments!
Download includes:
Easy to edit, fillable PDFs for four, five, six, and seven pill slot templates
Both 3 and 4 pill time periods/day templates are provided
Instructions
Sample daily pill schedule PDFs to follow format

4 pill time periods per day

3 pill time periods per day
Hope this makes medications easier!
♡S.S
You might also like
Fidgeting strategies & activities for Lewy Body Dementia
Fidgeting is a common symptom of Lewy Body Dementia, and it can be quite challenging to manage. Here are some fidget prevention strategies and activities that might help your loved one.
Fidget prevention strategies
When you LO fidgets, it is often a signal of restlessness, boredom, lack of purpose, or anxiety. Addressing these underlying issues can help reduce fidgeting, and these strategoes can help:
Exercise: Engaging in regular physical activity can help reduce restlessness and fidgeting. Aim for at least 150 minutes per week of moderate-intensity aerobic exercise, such as walking, physical therapy sessions, or a local Rock Steady Boxing class for Parkinson's. If balance is a problem, they might feel more comfortable using these under the desk stationary bike peddles which can easily be done at home.
Mindfulness: Practicing mindfulness techniques, like deep breathing, meditation, or yoga, can help increase their focus and calmness. It also a great activity to do together! Consider using a guided meditation apps or a guided meditation video on YouTube like the beach or floating on a cloud. You can stream YouTube on any Smart TV - or screen share it from your iPad or Phone - just remember to set the playback speed to .75 so it's not too fast.
Environmental modifications: Make sure your surroundings are comfortable and safe. Reduce clutter, provide adequate lighting, and maintain a comfortable temperature. You may also want to consider using a weighted blanket or weighted lap pad for deep pressure stimulation.
Scheduled activities Having a structured routine with scheduled activities can help reduce restlessness and fidgeting. This could include hobbies, social engagements, or simple tasks like sorting through photos or organizing drawers.
Distraction: Try engaging in an activity that requires your LO's full attention, such as reading, listening to music, or doing puzzles (Springbok has some good ones). This can help distract them from the urge to fidget.
Massage or Acupressure: A gentle hand or foot massage can help alleviate restlessness and promote relaxation. Alternatively, you can focus on these acupressure points which helps reduce their anxiety and calm them. Consider seeking the help of a professional massage therapist or enlisting the support of a caregiver for regular massages.
Medication: In some cases, medications such as antipsychotics or antidepressants may be prescribed to help manage restlessness and fidgeting associated with Lewy Body Dementia. It's important to discuss this option with your healthcare provider.
Fidgeting activities
It's a good idea to have some activities on hand for your LO when they fidget. Please keep in mind that everyone is unique, and you know your LO best, so tailor activities to their skills and interests.Here a few fidgeting activities for my mom at various stages to give you some examples:
Eating a bowl of pistachio nuts in shells to keep her hands busy
Folding paper or napkins is something Mom enjoys doing now. We started doing Origami together as a fun activity after snack time in the afternoon. We don't do any complicated origami projects (mostly for my benefit!), and when Mom is having a hard day, I fold the paper, and let her smooth out the creases.
Pairing colored socks or colored washcloths and then folding them
A 24" string of paracord rope with several knots tied into the string. I would ask Mom to help me get the knots out, and she was - as always! - happy to help.
Sorting coins from a change jar
Looking at fabric swatches or a color fan deck for a "design" project around the house.
Measuring spices for recipes or sorting/smelling the spices while we're cooking in the kitchen.
Petting her Joy For All Pet Companion ("Miss Kitty").
It's important to remember to be flexible. What works one day may not work the next, so learn to adapt and try something else.
Hope this helps!
♡S.S
You might also like
How to clean urine
out of couch, carpet, bedding, and mattress
Urinary incontinence is quite common with Lewy Body Dementia. Especially as the disease progresses. This post offers tips to prepare you for potential accidents so you can handle them with ease.I know caregiving is exhausting and cleaning up urine is not fun, but it's important to stay calm when accidents occur. The last thing you'd want is to cause further distress to your loved one or deepen their feelings of shame or embarrassment over something beyond their control.Treat it as no big deal, and just clean it up with these tips below.
Couch (or any upholstered furniture)
What you'll need:
- 3 microfiber cloths
- 1 regular cloth
- 1 tablespoon dishwashing liquid
- 2 cups of cold water
- 1 tablespoon white vinegar
- 1 small bowl
Instructions:Gently dab fresh urine stain with a clean, dry microfiber cloth to absorb excess liquid. Avoid rubbing, which can spread the stain.Next, in a small bowl, mix one tablespoon of dishwashing liquid and two cups of cold water. Add one tablespoon of vinegar to disinfect and neutralize odors. Stir gently so it doesn't get sudsy.Dip a new microfiber cloth in the solution and carefully blot the stain from the edges inward. Repeat as needed.Then rinse with a damp cloth to remove detergent residue.Finally, gently pat dry with another clean, dry microfiber cloth until no moisture remains.
To Prevent Future Urine Stains:Place a Washable 34" x 36" Incontinence Bed Pad on your sofas and chairs underneath your loved one. If the pad gets wet, simply toss it in the washing machine.
Carpet
What you'll need:
- 1/3 cup of distilled white vinegar
- 1/4 cup baking soda
- 1/4 cup mild dish soap
- 1 cup water
- Spray bottle
- Paper towels or 3 clean washcloths
Instructions:Soak up as much urine as possible using paper towels or a clean clothRinse the stain once with cold water.Blot with paper towels or clean cloth to remove excess waterCombine 1/3 cup of distilled white vinegar, 1/4 cup baking soda, 1/4 cup mild dish soap, and 1 cup water into a spray bottle and shake well.Spray soiled area with your solution, dab it with some clean paper towels or a washcloth, and allow it to sit for at least fifteen minutes.Blot the area with a clean washcloth to remove the liquid, and let it dry.If the urine smell isn't gone, repeat the two steps above.Once the odor is gone, vacuum up any residue.
Bedding
What you'll need:
-1 cup of distilled white vinegar
Instructions:Place your bedding in the washing machine, turn the water temp to cold, and add one cup of distilled white vinegar. Run a full wash-cycle - without detergent - to allow the vinegar solution to fully penetrate the fibers.Once the full wash cycle is complete, add your laundry detergent, and run again with warm water.BTW, this method also works for clothing.
To Prevent Future Urine Stains:We recommend using a 18" x 24" Washable Bed Pad underneath your LO at night along with a good pair of incontinence underwear. Position the pad between their lower back and upper thighs to contain urine to that area.You should also invest in a good mattress protector to go under the fitted sheet to prevent urine from soaking their mattress. As you'll see below, mattress stains are the hardest to clean, so a washable mattress protector is a must-have.
Mattress
What you'll need:
- Distilled white vinegar
- Water
- 1/4 cup baking soda
- Spray bottle
- 2-3 small towels (washcloth or hand towels)
- Vacuum hose (or hand-held Dustbuster)
Instructions:Step 1: Start by removing all your bedding and tossing it in the wash.Step 2: Grab a spray bottle and fill it halfway with white vinegar, then top it off with water.Step 3: Use a dry towel to blot the urine on the mattress. Avoid scrubbing to prevent pushing the urine deeper into the foam, which could make it trickier to remove the odor.Step 4: Once you've blotted most of the moisture, generously spray the white vinegar mixture over the area. Keep blotting to remove any excess liquid.Step 5: Sprinkle baking soda over the area and leave it for 8-10 hours, or longer if possible.Step 6: Vacuum up the baking soda and check the spot. If there's still a stain or odor, repeat the process until your mattress is fresh and clean again.
To Prevent Future Urine Stains:Again, buy a mattress protector and some washable bed pads to spare yourself any future hassle.
Fingers crossed you won't
need these tips again!
♡S.S
You might also like
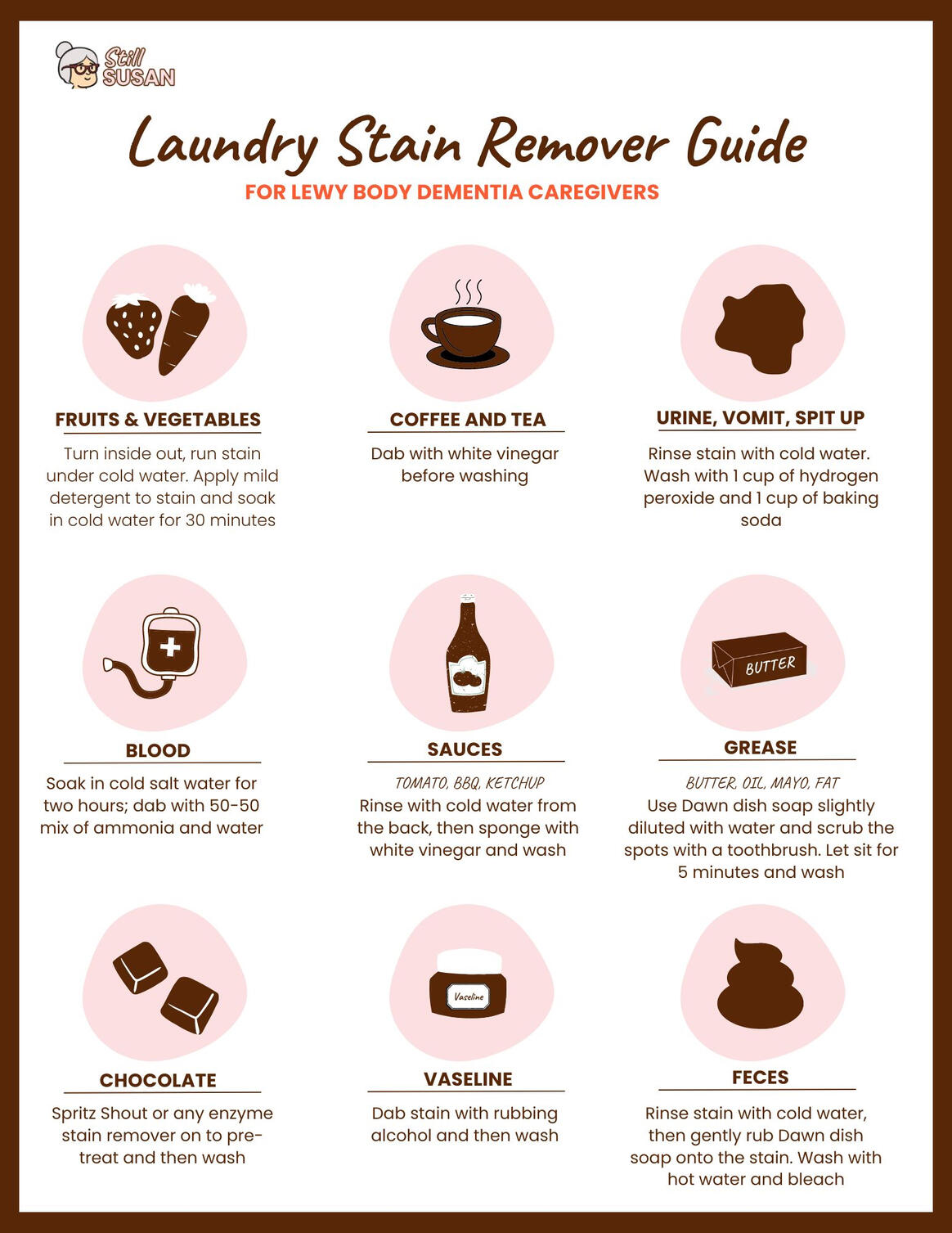
FREE DOWNLOAD
Laundry stain remover guide for Lewy Body Dementia caregivers
As caregivers, one common issue you might come across is dealing with laundry stains caused by spills or accidents. That's why we've put together this handy laundry stain remover guide to help you tackle those pesky stains like a pro. From removing grease and sauce stains to dealing with urine or poop, we've got you covered with this printable, time-saving guide.

FREE DOWNLOAD
Laundry Stain Remover
Guide for Lewy Body
Dementia caregivers
Slay those stains, caregivers!
♡S.S
You might also like
Pressure sore prevention for Lewy Body Dementia
People with Lewy Body Dementia can be more likely to develop pressure sores in the later stages. This often happens due to challenges like reduced circulation, decreased mobility, and difficulty moving independently, which can lead to prolonged pressure on certain areas like elbows, heels, and hips. Additionally, skin deterioration from urinary incontinence can create uncomfortable pressure ulcers on the buttocks.Because it can be hard for your loved one to express their discomfort or pinpoint where they’re feeling pain, it’s really important for caregivers to monitor their skin closely. The last thing anyone wants is for a pressure sore to get severely infected, which could lead to a lot of discomfort and agitation for your loved one. Not to mention, treating those sores can be quite a handful for you, so it’s definitely best to take steps to prevent them.
Pressure sore prevention strategies
Early detection: This is key to preventing pressure sores from worsening and becoming infected. And from experience, I can tell you that a bad pressure sore can appear out of nowhere in a few days, so keep a close eye out for them. Regularly check the skin for redness, swelling, or changes in texture, and report any concerns to healthcare professionals for further evaluation.
Regular repositioning: Change positions frequently to relieve pressure on their skin. This can be done by shifting their weight every 15-30 minutes, using a small wedge pillow, rolled up towel, or cushions to support vulnerable areas, and ensuring that individuals have proper seating and bedding arrangements.
Keep the skin clean and dry: Gently clean and moisturize the skin regularly, paying special attention to areas prone to pressure sores like the buttocks and heels. Avoid using harsh chemicals or abrasive materials on the skin, as this can exacerbate the risk of developing pressure sores.
Protect the skin from incontinence: As soon as your LO becomes regularly incontinent, caregivers should make sure to add a barrier cream to the buttocks throughout the day and at night to keep the skin protected from urine and feces.
We use petroleum jelly during the day and a 50-50 mixture of petroleum jelly and Desitin overnight to protect the skin after every cleaning. I know it's a lot of extra work, but pressure sores on the tush are hard to heal, and cause a great deal of discomfort for your LO, so it's worth the effort.Keep weight off of problem areas: For areas that are prone to pressure sores, I found that both heel protectors and sleeping on an air pressure mattress pad at night have been highly effective for warding off sores....and keeping Mom pain-free and comfy so she can sleep through the night. If your LO is prone to heel sores, you can also put a pillow under the feet with the heels hanging over the edge so they are not touching the surface.
Proper nutrition and hydration: A balanced diet rich in vitamins and minerals, as well as plenty of water, can help maintain healthy skin and prevent pressure sores from developing.
Regular exercise and physical activity: Gentle movements and exercises to improve circulation and prevent skin breakdown. This can include activities such as stretching, walking, and gentle yoga, which can help maintain skin integrity and reduce the risk of pressure sores.
Supplies to help prevent pressure sores
Keep these supplies on hand to help manage any emerging pressure sores:
Petroleum Jelly: A petroleum jelly like Vaseline is used to keep the pressure sore moist or as a barrier cream on the buttocks to prevent urine or stool from penetrating the skin. To prevent pressure sores on the buttocks, smear petroleum jelly over the area after every daytime cleaning.
Zinc Oxide Cream: A zinc oxide cream (we use Desitin) promotes healing, lessens inflammation, and disinfects. To prevent pressure sores on the buttocks overnight, do a 50-50 mixture of zinc oxide and petroleum jelly and smear it on the buttocks after washing the area.
Manuka Honey: When an emerging pressure sore is REALLY red, we found that Manuka honey works well. Manuka has antibacterial, antiviral, anti-inflammatory, and antioxidant properties which can be used to treat wounds and skin ulcers, according to research.
Non-stick pad with adhesive tabs: These pads keep the pressure sore covered to avoid friction and keeps the sore moist to speed up the healing process. I use the Equate brand from Walmart, but Curad works just as well.
Paper Tape: This gentle, breathable tape holds securely and removes easily so it won't irritate delicate or fragile skin. It also won't cause pain to your LO when removing, more importantly. Again, I use the paper tape from Equate since it's cheap and easy to get with the rest of my Walmart deliveries
What to do when you see a potential pressure sore?
Heel, Elbow, and Hips:
If you see a slight red spot, gently wash the area with mild soap and pat it dry. Apply a dime-size amount of petroleum jelly (or Manuka honey) with a clean finger, rubber glove, or popsicle stick, and then cover the wound with a non-stick pad with adhesive tabs and paper tape.Repeat this process daily for a week or so until the red spot disappears. If it starts to get worse or becomes dark red, call your doctor and ask for a wound care specialist referral.
Buttocks:
In addition to relieving pressure on the affected area, keeping the emerging pressure sore clean and applying a barrier mixture is essential.Start by gently cleaning the red spot with some mild soap and water, then pat it dry. Create a 50-50 mixture of petroleum jelly and zinc oxide cream (like Desitin). Apply this mixture to the buttocks using a popsicle stick, rubber glove, or clean finger every time you clean and change their incontinence briefs to protect their skin.It should take about a week for the red spot to disappear. But again, if the pressure sore gets worse or becomes dark red, call your doctor to get a wound care specialist referral.
"An ounce of prevention is worth a pound of cure." - Benjamin Franklin
♡S.S
You might also like
How to handle common Lewy Body Dementia behavioral problems
Handling common Lewy Body Dementia behavioral issues can be challenging, but with patience and understanding, caregivers can help their loved ones manage their symptoms effectively.It should be noted that if your loved one is exhibiting extreme or abnormal behavioral changes for a few days, it may be a Urinary Tract Infection (UTI), and you should contact their doctor.
Hallucinations and delusions
Lewy Body hallucinations can often lead to experiencing sights or sounds that aren’t really there, while delusions involve a strong belief in something that isn’t true, despite evidence to the contrary. Both of these symptoms are frequently seen in individuals with LBD.As a caregiver, it’s important to create a calm and reassuring environment during these moments. It’s best to avoid arguing or trying to correct them about their experiences, as this might increase their agitation. Instead, acknowledge their feelings and perceptions, whether they are amusing, strange, or frightening, and respond in a way that validates their emotions. This approach can help ease the situation and provide comfort.Consult with a healthcare professional about possible medication adjustments to help manage these symptoms.
Fluctuating awareness and attention.
Caregivers can help their LO by maintaining consistent routines and schedules to reduce confusion and disorientation. It is also important to provide a safe environment with minimal distractions to help with their attention span. Encouraging regular exercise and engaging in stimulating activities can also help improve cognitive function and overall well-being.
Agitation and aggression
Agitation and aggression are also common behavioral issues in individuals with Lewy Body Dementia. Caregivers should try to identify triggers that may be causing these behaviors and work to address them. Pain, discomfort, hunger, frustration, boredom, a noisy or overstimulating environment, or even something you did (unintentionally, of course) are common triggers.Redirecting their attention to a calming activity or using relaxation techniques such as deep breathing exercises can help reduce agitation. When dealing with aggression, it is extremely important for caregivers to stay calm and patient, and seek help from healthcare professionals if necessary.
Sleep disturbances
Sleep disturbances are a common issue in individuals with Lewy Body Dementia. Caregivers can help by establishing a consistent bedtime routine and creating a soothing sleep environment. My mom, for example, sleeps on an alternating air pressure mattress to keep her comfortable, listens to "Healing Sounds" or "Babbling Brook" on Alexa, and gets a 5 minute mini-massage before bed every night from my dad. This routine has been working for awhile (fingers crossed!), and she's able to sleep through the night. You know your LO better than anyone else, so figure out a soothing environment and routine that works best for them.Limiting caffeine and alcohol intake, as well as engaging in regular physical activity during the day, can also help improve sleep quality. If sleep disturbances persist, it is important to consult with a healthcare professional to explore potential medication options.
Handling common behavioral issues in individuals with Lewy Body Dementia requires patience, understanding, and a proactive approach to provide the best possible care for your LO. It's takes a lot of work - and it's exhausting - but keeping your LO feeling safe and comfortable is well worth it.
Hope these help your loved one!
♡S.S
You might also like
Types of finger food to eat for late stage Lewy Body Dementia
It’s important to let your loved one maintain control and independence, and eating is no exception. Below is a list of good finger food options to help set them up for success.A few tips for success:
Nothing too messy or crumbly to help them maintain their dignity and avoid frustration.
Keep in mind if crunchy or softer foods would suit them better if they have issues with teeth or swallowing, for example.
Watch the temperature. Make sure nothing is too hot or cold for your loved one to eat with their fingers.
Fruits & Vegetables
Apple - slices
Asparagus
Banana - whole or slices
Blackberries
Blueberries
Broccoli
Brussels Sprouts
Cantaloupe
Carrots - sticks or baby
Cauliflower
Celery
Cucumber - slices or sticks
Green Beans
Kiwi
Melon
Oranges
Pears
Pineapple
Strawberry
Watermelon
Breakfast
Bagels - cut into pieces
Banana Bread
Belvita Biscuits
Egg Bites
French Toast Sticks
Granola Bars - soft or chewy
Hash Browns - regular or sweet potato
Mini Quiches
Pancakes - cut into strips
Pumpkin Bread
Smoothies/ Protein shake
Toast - strips or quartered
Waffles - cut in strips
Wasa Crispbread - multi grain with cream cheese (Mom’s favorite!)
Lunch & Dinner
Boneless Wings
Cheese Cubes
Chicken Fingers or Nuggets
Deli Meat - rolled up with cheese
Deviled Eggs
Dumplings
Egg Bites
Empanadas
Fish Sticks
Garlic Bread
Grilled Cheese - quartered
Hard Boiled Eggs
Meatballs
Mini Muffin Tin Recipes
Mac & Cheese Bites
Mini Egg Rolls
Mini Quiches
Mozzarella Sticks
Pigs in a Blanket
Pizza - rolls, mini bagels or cut into small pieces
Potato Wedges
Quesadilla
Ravioli
Sandwich - cut into squares or wrap
Sliders
Spanakopita - rolls or triangles
String Cheese
Stuffed Grape Leaves
Sweet Potato Fries
Tater Tots
Veggie Patty
Veggie Tots
Dessert
Brownies
Cookies
Fruit Popsicles (Outshine is Susan’s fav)
Ice Cream - cone, popsicle, or sandwich
Mini Pastries
Pound Cake
Hope this helps!
♡S.S
You might also like
Tips to manage incontinence for Lewy Body Dementia
Lewy Body Dementia can cause a variety of symptoms, including incontinence. Incontinence refers to the inability to control one's bladder or bowels, leading to leaks or accidents. Dealing with incontinence can be challenging, but there are some tips and strategies that can help your loved one with Lewy Body Dementia manage this symptom and help them maintain their quality of life.
In the event of an accident, remain calm.
How you treat your LO in these moments really matters. Although they might not recall your exact words, they'll remember how you made them feel.Particularly in the beginning, your LO with LBD could feel humiliated about their incontinence problems. To ease their anxiety and preserve your relationship and trust, it's critical to provide comfort, empathy, and an upbeat attitude.Tell them "everyone does it," or share a personal story of when you peed yourself. In either case, remain calm, tidy up the accident, and move on.
Regular bathroom breaks
It's important to establish a routine for bathroom breaks. Setting regular times throughout the day for bathroom visits can help to minimize accidents and improve bladder control. It may also be helpful to remind the individual to use the bathroom regularly, as memory and cognitive issues associated with Lewy Body Dementia can make it easy to forget.Also, add signage to the front of your bathroom doors. A picture of a toilet and the word "bathroom" will help them easily identify where to go, especially in a hurry.
Easy and safe bathroom access
Another helpful tip is to make sure that the individual has easy access to the bathroom. This may involve removing obstacles or clutter in the home that could make it difficult for the individual to reach the bathroom quickly. You should also provide adequate lighting at night. In the bathroom, installing handrails or grab bars near the toilet can provide much-needed support and stability for individuals with Lewy Body Dementia who may have difficulty walking or maintaining balance. We installed a bathroom safety bar next to the toilet for Mom, and a toilet riser seat is also a good idea if it's hard to get up and down.
Clothing
It is also important to provide the individual with clothing that is easy to remove and wash in case of accidents. Clothing with elastic waistbands or Velcro closures can make it easier for the individual to change quickly if needed. It may also be helpful to keep a supply of extra underwear, pants, and incontinence products on hand in case of accidents if you're out.
Incontinence products
Incontinence underwear and briefs help individuals with Lewy Body Dementia keep their dignity and independence by preventing leaks and giving them a sense of security. Understandably, your LO might be hesitant to use incontinence products at first. If you encounter any resistance, try not to pressure them. They'll eventually come around in their own time.A few tips for incontinece products:• Avoid calling them "diapers." For them, incontinence is a delicate subject and could even be mortifying. Instead them "briefs," "underpants," "fancy pants," or any other term you like instead of the dreaded D-word. Maintaining their dignity is what matters most.• For a good, cost-efficient incontinence products, the Assurance brand from Walmart is great. If you're willing to spend more, check out the Because products which people seem to love.• Sign-up for auto-delivery (Amazon and Walmart) or subscription services where possible so you have one less thing you have to do. And keep an extra pack on hand in case of shipping delays or if you run out between shipments.
Protect your bed & furniture
Cleaning urine is exhausting, and quite frankly, as a full-time caregiver you don't have time for it. Save yourself a lot of hassle and get washable protection pads for your bed and furniture, and a good mattress protector. We use the 18" x 24" washable pad under Mom's bottom area at night in bed, and the 34" x 36" washable pad for chairs and furniture. To protect the bed, we bought this washable mattress protector to keep urine from penetrating the mattress.
Ask your doctor for medications
In some cases, medication may be necessary to help manage incontinence. Talk to a healthcare provider about potential treatment options for incontinence, as certain medications may be helpful in improving bladder control.
Hope these tips help!
♡S.S
You might also like
Songs to sing to your loved one with Lewy Body Dementia in the morning
There is something special about starting the day by singing to your loved one with Lewy Body Dementia. Despite the challenges they may face, music has a way of reaching past the barriers of memory loss and confusion, allowing for moments of a sweet connection.Singing to them not only provides emotional soothing but also triggers positive brain responses that can improve their mood and cognitive function. So, even if you're a not-so-great singer like me, don't hesitate to start each day on a good note by singing softly to your loved one living with Lewy Body Dementia.Here are my mom's favorite morning songs (and links to lyrics), which you are free to use.
"Three Little Birds"
"You Are My Sunshine"
"Somewhere Over the Rainbow"
"Good Morning"
"What a Wonderful World"
Enjoy this day with your loved one!
♡S.S
You might also like
Easy blender drink recipes for hydration
Dehydration is common with the later stages of Lewy Body Dementia patients due to forgetfulness, and in some cases, the ability to recognize when they’re thirsty.In Mom’s case, the taste of water no longer appealed to her, so I got out the blender and concocted a few easy drinks to help her stay hydrated during the day.Below are her favorite cocktails, and I hope they help your loved one stay hydrated, too.
Lemon, Ginger, & Honey:
2 cups (16oz) cold water
2 tablespoons of Lemon Juice (freshly squeezed or concentrated)
1 tablespoon Honey
1 tablespoon GingerPut all ingredients in a blender on high until ginger is finely chopped and fully blended. If the chunks are too big, strain before serving.
Apple Juice & Ginger:
2 cups (16oz) cold water
1 cup (8oz) of their favorite 100% apple juice (Honeycrisp Apple is Mom’s favorites)
1 tablespoon gingerPut all ingredients in a blender on high until ginger is finely chopped and fully blended. If ginger chunks are still too big, strain before serving.
Lime, Pineapple, & Ginger:
2 cups (16oz) cold water
1/2 cup (4oz) 100% Pineapple Juice
1 tablespoon Lime juice
1 tablespoon GingerPut all ingredients in a blender on high until ginger is finely chopped. If ginger chunks are still too big, strain before serving.
Passion Fruit Juice & Mint:
2 cups (16oz) cold water
1 cup (8oz) Ceres 100% Passion Fruit Juice or Passion Fruit Frozen chunks
4 whole mint leaves (no stems)
1 splash of lime juice (optional)Put all ingredients in a blender on high until mint is finely chopped and fully blended. If the mint or passion fruit chunks are still too big, strain before serving. Feel free to add more mint leaves to your liking or more Passion Fruit juice/chunks if you want it sweeter.
Cheers!
♡S.S
You might also like
High calorie, healthy smoothie recipes
The later stages Lewy Body Dementia can be incredibly challenging for both you and your loved one. One way to provide nourishment and hydration while also ensuring ease of consumption is by making smoothies, especially if your loved one doesn't like Boost or other artificial tasting protein shakes like mine.When chewing became too exhausting for my mom and she starting losing weight, I started making her these homemade smoothies every morning with no added preservatives, and sweetened only with a little honey.These smoothies have around 850+ calories per serving, and soon enough, Mom's weight began to climb back up.
Banana, Chocolate, & Peanut Butter Smoothie:
Ingredients:
1 cup unsweetened coconut, oat, or almond milk (any milk will do)
5-6 tablespoons all natural peanut butter
2 tablespoons honey (you can add more at the end if you want it sweeter)
1/2 cup uncooked rolled oats or instant oatmeal
1 teaspoon unsweetened cocoa powder
1 frozen banana (frozen makes it creamer)
6 ice cubes
Directions:
Blend coconut milk, peanut butter, and honey together (to save some time, double these ingredients and keep 1/2 in the fridge for the next day). Add in oatmeal and cocoa powder, and blend again until smooth. Finally, add in banana and ice cubes, and blend until smooth.FYI, if you're worried about oat chunks, strain the smoothie before serving.
Approximate calorie count:
873 calories
Peanut Butter & Jelly Smoothie:
Ingredients:
1 cup unsweetened coconut, oat, or almond milk (any milk will do)
5-6 tablespoons all natural peanut butter
2 tablespoons honey (add more at the end if you want it sweeter)
1/2 cup uncooked rolled oats or instant oatmeal
1/2 cup frozen blueberries
1/2 cup frozen whole strawberries
1 tablespoon (heaping) Smucker's Simply Fruit Seedless Red Raspberry Jam or 1/4 cup raspberries
3 ice cubesDirections:
Blend coconut milk, peanut butter, and honey together (to save some time, double these ingredients and keep 1/2 in the fridge for the next day).Add in oatmeal and frozen berries (or jam, if no raspberries), and blend until smooth. Finally, add ice cubes and blend again until smooth.FYI, if you're worried about seeds or oat chunks, strain the smoothie before serving.
Approximate calorie count:
923 calories
Apple & Peanut Butter Smoothie:
Ingredients:
1 cup unsweetened coconut, oat, or almond milk (any milk will do)
5-6 tablespoons all natural peanut butter
2 tablespoons honey (add more at the end if you want it sweeter)
2/3 cup uncooked rolled oats or instant oatmeal
1/2 teaspoon vanilla extract
1 teaspoon cinnamon
dash of nutmeg (optional)
1/2 cup apple sauce (I use unsweetened)
5 ice cubesDirections:
Blend coconut milk, peanut butter, and honey together (to save some time, double these ingredients and keep 1/2 in the fridge for the next day).Add in oatmeal, and blend again until smooth. Finally, add in the apple sauce and ice cubes, and blend until smooth.FYI, if you're worried about oat chunks, strain the smoothie before serving.
Approximate calorie count:
795 calories
Hope these recipes help!
♡S.S
You might also like
How to prevent constipation in Lewy Body Dementia care
Constipation is a common issue in individuals with Lewy Body Dementia, and it is important to take steps to prevent and manage it in order to maintain the overall health and comfort of your loved one. Constipation can also cause UTI's, which is something to keep in mind.Please note, these tips are for mild constipation. And, as always, consult with a doctor prior to using any product remedies mentioned below or if your loved one is experiencing severe or chronic constipation.
Healthy and balanced diet
A diet that is high in fiber, such as fruits, vegetables, whole grains, and legumes, can help to promote regular bowel movements and prevent constipation. This can be hard to achieve in the later stages of Lewy Body Dementia, so stick to foods that can easily be pureed or finely blended, like oatmeal.
Stay hydrated
It is also important to make sure that the individual is drinking an adequate amount of water and liquids each day, as dehydration can contribute to constipation. Adding soup to their diet is recommended, and foods like yogurt, fruit popsicles, jello, and ice cream are all also helpful foods for hydration in moderation.
Prune juice
Prune juice is a popular natural remedy for constipation, as it contains fiber and sorbitol which help promote bowel movements. By drinking prune juice daily, it can help soften stool and make it easier to pass, relieving constipation. Additionally, prune juice also contains antioxidants and vitamins that can improve overall digestive health.
Acacia Senegal Powder
Acacia Senegal Powder, derived from the sap of the Acacia Senegal tree, is known for its numerous health benefits, one of which includes its effectiveness in relieving constipation. This powder contains high amounts of soluble fiber, which helps to regulate bowel movements and improve overall digestive health. When taken regularly, Acacia Senegal Powder can soften stools, promote regularity, and reduce the discomfort associated with constipation. Additionally, this natural remedy is gentle on your LO's stomach and does not cause the harsh side effects often seen with traditional laxatives.
Heather's Tummy Care
Heather's Tummy Care for constipation is a game-changer when it comes to managing digestive issues. Designed with natural ingredients like organic ground flaxseed and acacia senegal fiber, this product helps promote healthy bowel movements, increases good gut flora, and relieves discomfort associated with constipation. It's gentle on the stomach, making it suitable for those with sensitive digestive systems. What sets Heather's Tummy Care apart is its focus on providing relief specifically for individuals dealing with IBS-related constipation, if your LO has a sensitive stomach.
Miralax
Miralax is a common over-the-counter medication used to treat constipation. You mix the powder with a glass of water or diluted juice. It works by drawing water into the colon, which softens the stool and makes it easier to pass. It's important to follow the instructions on the package and not take more than recommended.Some possible side effects include bloating, cramping, and gas. If constipation persists or worsens, it's best to consult a doctor for further advice.
Colace
Colace is a popular over-the-counter medication used to treat constipation. It's a stool softener AND a laxative, making it easier for your LO with Lewy body Dementia to expel poop in the later stages.It's important to follow the recommended dosage instructions and drink plenty of water while taking Colace to help it work effectively. And, again, please check with a healthcare professional before using.
Hope this is useful!
♡S.S
You might also like
Our Privacy
Policy
This document outlines the privacy policy for Still Susan, which utilizes Google Analytics to enhance user experience and analyze site performance. We are committed to safeguarding your privacy and ensuring that your personal information is handled responsibly.1. Information Collection: Our website collects data through Google Analytics, which may include information about your device, browser type, pages visited, and the time spent on our site. This data is collected anonymously and is used solely for analytical purposes.2. Use of Information: The information gathered through Google Analytics helps us understand user behavior and improve our website's functionality. We do not use this data to personally identify individual users.3. Cookies: Google Analytics employs cookies to collect data. You can manage your cookie preferences through your browser settings. However, disabling cookies may affect your experience on our website.4. Data Sharing: We do not sell or share your personal information with third parties. Google Analytics may process data in accordance with its own privacy policy.5. Changes to the Privacy Policy: We reserve the right to update this privacy policy as necessary. Any changes will be posted on this page, and we encourage you to review it periodically.By using our website, you consent to the collection and use of information in accordance with this policy. If you have any questions or concerns regarding our privacy practices, please contact us.